Prostatitis Treatment & Management
Treatment of prostatitis should be tailored to symptoms and culture findings and should be supportive. Suprapubic catheterization may be warranted in severe urinary obstruction and should be placed in consultation with a urologist. For further information, the European Association of Urology has treatment guidelines available on chronic pelvic pain and on prostatitis and chronic pelvic pain syndrome. [34, 38]
See the following for more information:
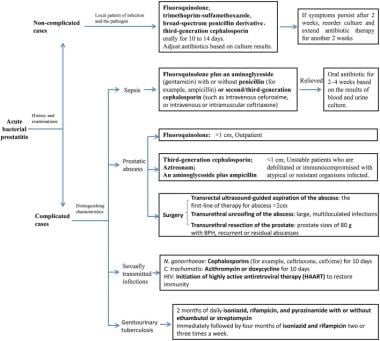
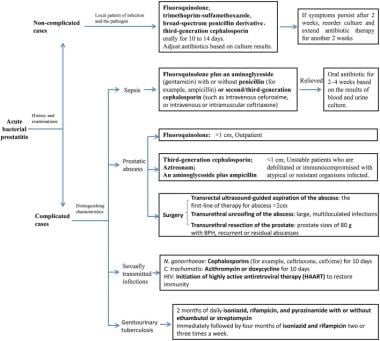
Acute Bacterial Prostatitis
Individuals with acute bacterial prostatitis who are acutely ill, have evidence of sepsis, are unable to voluntarily urinate or tolerate oral intake, or have risk factors for antibiotic resistance require hospital admission for parenteral antibiotics and supportive care. [39] Antibiotic therapy initially should include parental bactericidal agents such as fluoroquinolones, aminoglycosides with or without penicillin derivatives, and third-generation cephalosporins. [40]
Since April 2007, the Centers for Disease Control and Prevention (CDC) has no longer recommended fluoroquinolone antibiotics to treat gonorrhea in the United States. [41, 42] Current CDC treatment guidelines for gonococcal infection recommend single-dose IM ceftriaxone, plus single-dose oral azithromycin or 7 days of oral doxycycline. [42, 18] Co-treatment offers the benefits of hindering the development of antimicrobial resistant gonococci and covering C trachomatis, which often accompanies gonococcal infection.
Patients without a toxic appearance can be treated on an outpatient basis with a 28-day course of oral antibiotics, usually a fluoroquinolone or trimethoprim-sulfamethoxazole. Urologic follow-up is necessary to ensure eradication and to provide continuity of care to prevent relapse.
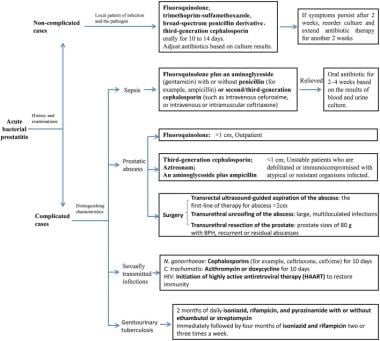
--> Treatment algorithm for acute bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Urinary retention may complicate acute infection and warrant hospitalization. Suprapubic catheters are considered safer than urethral catheterization in severe obstruction due to prostatic swelling from bacterial infection and may be placed in consultation with a urologist. [43]
Provide supportive measures such as antipyretics, analgesics, hydration, and stool softeners as needed. Urinary analgesics such as phenazopyridine and flavoxate are also commonly used.
Avoid serial examinations of the prostate to avoid seeding of the blood and bacteremia in acute bacterial prostatitis.
In cases of prostatic abscess, the fluctuant site may be drained under local anesthesia either transrectally or transperineally. When performed transperineally, a pigtail catheter can be inserted as a drain. Cystoscopic, transurethral unroofing of an abscess also is possible with the patient under anesthesia.
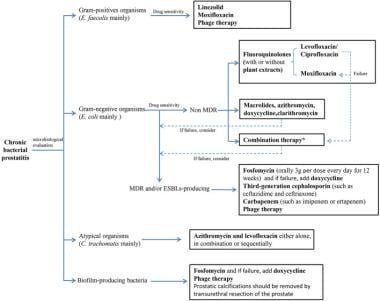
Chronic Bacterial Prostatitis and Pelvic Pain
A 4- to 6-week trial of antibiotic therapy is indicated in chronic bacterial prostatitis and chronic pelvic pain syndrome with inflammation, but no consensus exists regarding its use in chronic pelvic pain syndrome without inflammation and asymptomatic prostatitis. Recurrences of chronic bacterial prostatitis are common, possibly in part because few antibacterial agents distribute well into the prostatic tissue and achieve sufficient concentrations to eradicate infections. Preferred antimicrobial agents include fluoroquinolones, macrolides, tetracyclines, and trimethoprim. [44] Fluoroquinolones provide relief in about 50% of patients, and treatment is more effective if treatment starts earlier in the course of symptoms. The course of antibiotics can be repeated if the first course provides some relief. [45] A Cochrane review of 18 studies that compared the various fluoroquinolone antibiotics suggested that there were no differences in clinical efficacy or adverse events among them in treating chronic bacterial prostatitis. [44] Fosfomycin has been used to effectively treat multidrug-resistant gram-negative prostatitis. [46]
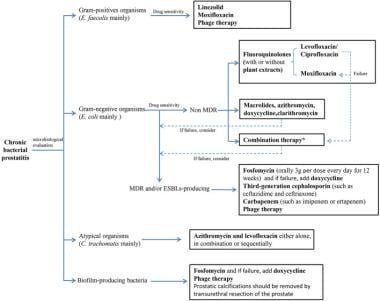
--> Treatment algorithm for chronic bacterial prostatitis. Courtesy of Frontiers Media [Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. Online at https://www.frontiersin.org/articles/10.3389/fphar.2020.00504/full].
Supportive measures such as analgesics (particularly nonsteroidal anti-inflammatory drugs [NSAIDs]), alpha-blocking agents, hydration, stool softeners, and sitz baths are often used. Alpha-blockers reduce bladder outlet obstruction and thus improve voiding dysfunction that may be associated with prostatic swelling that is common with prostatitis. [47]
Some evidence suggests that pelvic floor training/biofeedback can be effective in controlling the symptoms of chronic prostatitis and chronic pelvic pain syndrome. [21]
In cases where infected prostatic calculi serve as a nidus, transurethral resection or total prostatectomy may result in a cure.
If a patient has received no relief from antibiotics, NSAIDs, and alpha blockade, ensure prompt referral to a urologist.
Carefully treat associated septicemia in acutely ill patients. Carefully monitor for bladder outlet obstruction and renal failure. If urination issues do not resolve and incomplete emptying of bladder urine is suspected, refer the patient to a urologist for an evaluation of urination with flow rate and postvoid assessment of residual urine.
Chronic prostatitis/chronic pelvis pain syndrome (NIH Category III prostatitis) appears to be a collection of clinical phenotypes that may manifest as urinary symptoms, pain, sexual symptoms, and/or psychiatric issues. As a result, it largely has been resistant to monotherapy. Recently, a tailored multimodal approach to this condition has been advocated with success. Based on clinical phenotype, patients are placed into the "UPOINT" system, which classifies symptoms into urinary, psychological, organ-specific, infection, neurologic/systemic, and tenderness domains. [48] Based on the patient-specific symptom domains, multimodality therapy that is tailored to each patient is prescribed.
Prevention of Prostatitis
Protection against sexually transmitted diseases (STDs) also provides protection against many organisms associated with acute bacterial prostatitis, development of chronic prostatitis, and suspected causes of nonbacterial prostatitis.
Psychological stress has been associated with men who report symptoms of chronic prostatitis. [15, 4] Recognition of underlying psychosomatic disease in chronic cases and appropriate psychiatric referral and treatment lessen the recurrence rate.
Consultations
After primary management and stabilization of the patient with acute prostatitis, care is appropriately transferred to a urologist.
Aggressive treatment can lessen the chance of developing chronic prostatitis. Chronic bacterial prostatitis, chronic pelvic pain syndrome, and asymptomatic inflammatory prostatitis also are probably best treated by or in consultation with a urologist.
Notify the health department if a reportable STD is documented. Consult a psychiatrist if psychosomatic disorder is suspected.
Long-Term Monitoring
After initial improvement with parental antibiotics, acute bacterial prostatitis may be managed with outpatient care with a 2- to 4-week course of oral antibiotics and urologic follow-up. Management strategies for category II prostatitis, chronic bacterial prostatitis, include intraprostatic antibiotic injection, alpha-blocker therapy, transurethral resection of the prostate (TURP), and long-term antimicrobial suppression.
Additional therapeutic modalities studied for category III prostatitis include anti-inflammatories, phytotherapy, biofeedback, thermal therapy, and pelvic floor exercises.
Prostate-specific antigen (PSA) levels may be elevated with both prostatitis and prostate cancer. However, PSA levels typically fall after resolution of prostatitis but do not fall with prostate cancer. Patients found to have elevated PSA levels should have follow-up by their primary care physician, urologist, or both.
PSA levels may increase with acute prostatitis; with appropriate antibiotic treatment, levels usually return to normal within 1-3 months. [49] In some studies, a longer course of antibiotics has been shown to result in a decrease in PSA values in patients with category IV prostatitis.
References
- Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236-7. [QxMD MEDLINE Link].
- Davis NG, Silberman M. Bacterial Acute Prostatitis. 2022 Jan. [QxMD MEDLINE Link]. [Full Text].
- Motrich RD, Salazar FC, Breser ML, Mackern-Oberti JP, Godoy GJ, Olivera C, et al. Implications of prostate inflammation on male fertility. Andrologia. 2018 Dec. 50 (11):e13093. [QxMD MEDLINE Link].
- Berghuis JP, Heiman JR, Rothman I, Berger RE. Psychological and physical factors involved in chronic idiopathic prostatitis. J Psychosom Res. 1996 Oct. 41(4):313-25. [QxMD MEDLINE Link].
- Aaron LA, Herrell R, Ashton S, Belcourt M, Schmaling K, Goldberg J, et al. Comorbid clinical conditions in chronic fatigue: a co-twin control study. J Gen Intern Med. 2001 Jan. 16 (1):24-31. [QxMD MEDLINE Link].
- Khan FU, Ihsan AU, Khan HU, Jana R, Wazir J, Khongorzul P, et al. Comprehensive overview of prostatitis. Biomed Pharmacother. 2017 Oct. 94:1064-1076. [QxMD MEDLINE Link].
- Fu W, Zhou Z, Liu S, Li Q, Yao J, Li W, et al. The effect of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) on semen parameters in human males: a systematic review and meta-analysis. PLoS One. 2014. 9 (4):e94991. [QxMD MEDLINE Link].
- Rivero VE, Motrich RD, Maccioni M, Riera CM. Autoimmune etiology in chronic prostatitis syndrome: an advance in the understanding of this pathology. Crit Rev Immunol. 2007. 27 (1):33-46. [QxMD MEDLINE Link].
- Lampiao F, du Plessis SS. TNF-alpha and IL-6 affect human sperm function by elevating nitric oxide production. Reprod Biomed Online. 2008 Nov. 17 (5):628-31. [QxMD MEDLINE Link].
- Motrich RD, Salazar FC, Breser ML, Mackern-Oberti JP, Godoy GJ, Olivera C, et al. Implications of prostate inflammation on male fertility. Andrologia. 2018 Dec. 50 (11):e13093. [QxMD MEDLINE Link].
- Habermacher GM, Chason JT, Schaeffer AJ. Prostatitis/chronic pelvic pain syndrome. Annu Rev Med. 2006. 57:195-206. [QxMD MEDLINE Link].
- Taoka R, Kakehi Y. The influence of asymptomatic inflammatory prostatitis on the onset and progression of lower urinary tract symptoms in men with histologic benign prostatic hyperplasia. Asian J Urol. 2017 Jul. 4 (3):158-163. [QxMD MEDLINE Link].
- Nickel JC. Prostatitis. Can Urol Assoc J. 2011 Oct. 5 (5):306-15. [QxMD MEDLINE Link].
- Stancik I, Lüftenegger W, Klimpfinger M, Müller MM, Hoeltl W. Effect of NIH-IV prostatitis on free and free-to-total PSA. Eur Urol. 2004 Dec. 46 (6):760-4. [QxMD MEDLINE Link].
- Mastroianni A, Coronado O, Manfredi R, Chiodo F, Scarani P. Acute cytomegalovirus prostatitis in AIDS. Genitourin Med. 1996 Dec. 72(6):447-8. [QxMD MEDLINE Link].
- Gebo KA. Prostatic tuberculosis in an HIV infected male. Sex Transm Infect. 2002 Apr. 78(2):147-8. [QxMD MEDLINE Link].
- Krieger JN, Dobrindt U, Riley DE, Oswald E. Acute Escherichia coli prostatitis in previously health young men: bacterial virulence factors, antimicrobial resistance, and clinical outcomes. Urology. 2011 Jun. 77(6):1420-5. [QxMD MEDLINE Link].
- Brede CM, Shoskes DA. The etiology and management of acute prostatitis. Nat Rev Urol. 2011 Apr. 8(4):207-12. [QxMD MEDLINE Link].
- Barash A, Stern E, Hoelle R. A Case Report of Acute Prostatitis Secondary to Use of P-valve Condom Catheter During Cave Diving. Clin Pract Cases Emerg Med. 2021 Nov. 5 (4):436-439. [QxMD MEDLINE Link].
- Feneley M, Kirby RS, Parkinson C. Clinico-pathological findings simulating prostatic malignancy following sclerotherapy: a diagnostic pitfall. Br J Urol. 1996 Jan. 77(1):157-8. [QxMD MEDLINE Link].
- Murphy AB, Macejko A, Taylor A, Nadler RB. Chronic prostatitis: management strategies. Drugs. 2009. 69(1):71-84. [QxMD MEDLINE Link].
- Rees J, Abrahams M, Doble A, Cooper A, Prostatitis Expert Reference Group (PERG). Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU Int. 2015 Oct. 116 (4):509-25. [QxMD MEDLINE Link].
- Collins MM, Stafford RS, O'Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998 Apr. 159(4):1224-8. [QxMD MEDLINE Link].
- Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001 Mar. 165(3):842-5. [QxMD MEDLINE Link].
- Schaeffer AJ. Clinical practice. Chronic prostatitis and the chronic pelvic pain syndrome. N Engl J Med. 2006 Oct 19. 355(16):1690-8. [QxMD MEDLINE Link].
- Ku JH, Kim SW, Paick JS. Epidemiologic risk factors for chronic prostatitis. Int J Androl. 2005 Dec. 28 (6):317-27. [QxMD MEDLINE Link].
- Awadh B, Watson K, Abdou NI. Wegener prostatitis presenting with acute urinary retention. J Clin Rheumatol. 2006 Feb. 12(1):50-1. [QxMD MEDLINE Link].
- Huong DL, Papo T, Piette JC, Wechsler B, Bletry O, Richard F, et al. Urogenital manifestations of Wegener granulomatosis. Medicine (Baltimore). 1995 May. 74(3):152-61. [QxMD MEDLINE Link].
- Middleton G, Karp D, Lee E, Cush J. Wegener's granulomatosis presenting as lower back pain with prostatitis and ureteral obstruction. J Rheumatol. 1994 Mar. 21(3):566-9. [QxMD MEDLINE Link].
- Davis NG, Silberman M. Bacterial Acute Prostatitis. 2022 Jan. [QxMD MEDLINE Link]. [Full Text].
- Perletti G, Trinchieri A, Stamatiou K, Magri V. Safety considerations with new antibacterial approaches for chronic bacterial prostatitis. Expert Opin Drug Saf. 2022 Feb. 21 (2):171-182. [QxMD MEDLINE Link].
- Khattak AS, Raison N, Hawazie A, Khan A, Brunckhorst O, Ahmed K. Contemporary Management of Chronic Prostatitis. Cureus. 2021 Dec. 13 (12):e20243. [QxMD MEDLINE Link].
- Donovan DA, Nicholas PK. Prostatitis: diagnosis and treatment in primary care. Nurse Pract. 1997 Apr. 22(4):144-6, 149-56. [QxMD MEDLINE Link].
- [Guideline] Grabe M, Bishop MC, Bjerklund-Johansen TE, et al. Prostatitis and chronic pelvic pain syndrome. Guidelines on the management of urinary and male genital tract infections. Arnhem, The Netherlands: European Association of Urology (EAU). 2008 Mar. 79-88. [Full Text].
- McNaughton Collins M, MacDonald R, Wilt TJ. Diagnosis and treatment of chronic abacterial prostatitis: a systematic review. Ann Intern Med. 2000 Sep 5. 133(5):367-81. [QxMD MEDLINE Link]. [Full Text].
- Loeb S, Gashti SN, Catalona WJ. Exclusion of inflammation in the differential diagnosis of an elevated prostate-specific antigen (PSA). Urol Oncol. 2009 Jan-Feb. 27(1):64-6. [QxMD MEDLINE Link].
- de la Rosette JJ, Giesen RJ, Huynen AL, Aarnink RG, van Iersel MP, Debruyne FM, et al. Automated analysis and interpretation of transrectal ultrasonography images in patients with prostatitis. Eur Urol. 1995. 27(1):47-53. [QxMD MEDLINE Link].
- [Guideline] Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. General treatment of chronic pelvic pain. Guidelines on chronic pelvic pain. Arnhem, The Netherlands: European Association of Urology (EAU). 2008 Mar. 84-97. [Full Text].
- Coker TJ, Dierfeldt DM. Acute Bacterial Prostatitis: Diagnosis and Management. Am Fam Physician. 2016 Jan 15. 93 (2):114-20. [QxMD MEDLINE Link].
- Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, et al. Pharmacological Interventions for Bacterial Prostatitis. Front Pharmacol. 2020. 11:504. [QxMD MEDLINE Link].
- Centers for Disease Control and Prevention. Update to CDC's sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007 Apr 13. 56(14):332-6. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010 Dec 17. 59:1-110. [QxMD MEDLINE Link]. [Full Text].
- Yoon BI, Han DS, Ha US, Lee SJ, Sohn DW, Kim HW. Clinical courses following acute bacterial prostatitis. Prostate Int. 2013. 1(2):89-93. [QxMD MEDLINE Link].
- Perletti G, Marras E, Wagenlehner FM, Magri V. Antimicrobial therapy for chronic bacterial prostatitis. Cochrane Database Syst Rev. 2013 Aug 12. CD009071. [QxMD MEDLINE Link].
- Le BV, Schaeffer AJ. Genitourinary pain syndromes, prostatitis, and lower urinary tract symptoms. Urol Clin North Am. 2009 Nov. 36(4):527-36, vii. [QxMD MEDLINE Link].
- Grayson ML, Macesic N, Trevillyan J, Ellis AG, Zeglinski PT, Hewitt NH, et al. Fosfomycin for Treatment of Prostatitis: New Tricks for Old Dogs. Clin Infect Dis. 2015 Oct 1. 61 (7):1141-3. [QxMD MEDLINE Link].
- Nickel JC. alpha-Blockers for Treatment of the Prostatitis Syndromes. Rev Urol. 2005. 7 Suppl 8:S18-25. [QxMD MEDLINE Link]. [Full Text].
- DeWitt-Foy ME, Nickel JC, Shoskes DA. Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Eur Urol Focus. 2018 Sep 8. [QxMD MEDLINE Link].
- Sindhwani P, Wilson CM. Prostatitis and serum prostate-specific antigen. Curr Urol Rep. 2005 Jul. 6(4):307-12. [QxMD MEDLINE Link].
- Zhang ZC, Jin FS, Liu DM, Shen ZJ, Sun YH, Guo YL. Safety and efficacy of levofloxacin versus ciprofloxacin for the treatment of chronic bacterial prostatitis in Chinese patients. Asian J Androl. 2012 Nov. 14 (6):870-4. [QxMD MEDLINE Link].
- Mehik A, Hellström P, Sarpola A, Lukkarinen O, Järvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001 Jul. 88(1):35-8. [QxMD MEDLINE Link].
- Wise GJ, Shteynshlyuger A. How to diagnose and treat fungal infections in chronic prostatitis. Curr Urol Rep. 2006. 7(4):320-8. [QxMD MEDLINE Link].
- Kim JW, Oh MM, Bae JH, Kang SH, Park HS, Moon du G. Clinical and microbiological characteristics of spontaneous acute prostatitis and transrectal prostate biopsy-related acute prostatitis: Is transrectal prostate biopsy-related acute prostatitis a distinct acute prostatitis category?. J Infect Chemother. 2015 Jun. 21 (6):434-7. [QxMD MEDLINE Link].
- Etienne M, Pestel-Caron M, Chapuzet C, Bourgeois I, Chavanet P, Caron F. Should blood cultures be performed for patients with acute prostatitis?. J Clin Microbiol. 2010 May. 48 (5):1935-8. [QxMD MEDLINE Link].
- Gill BC, Shoskes DA. Bacterial prostatitis. Curr Opin Infect Dis. 2016 Feb. 29 (1):86-91. [QxMD MEDLINE Link].
- Breyer BN, Van den Eeden SK, Horberg MA, Eisenberg ML, Deng DY, Smith JF, et al. HIV status is an independent risk factor for reporting lower urinary tract symptoms. J Urol. 2011 May. 185 (5):1710-5. [QxMD MEDLINE Link].
Media Gallery
Bacterial prostatitis. Expressed prostatic fluid contains more than 10 white blood cells per high-power field, indicating prostatitis.
A nonspecific mixed inflammatory infiltrate that consists of lymphocytes, plasma cells, and histiocytes is typical in chronic bacterial prostatitis.
Urine culture with greater than 100,000 colony-forming units (CFU) of Escherichia coli, the most common pathogen in acute and chronic prostatitis. Chronic bacterial prostatitis must be confirmed and diagnosed using a urine culture.